Volumen 30, Nº 1 | 2012
Dieulafoy’s lesion of the terminal ileum -
Domingo Balderramo, Orlando García-Bosch, Anna Bargalló, Merce Navarro, Marta Martín, Alejandro Blasco and Alfredo Mata.
Palabras clave:
Keywords:
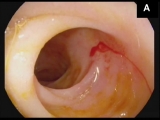
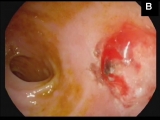
A 58-year-old man was admitted to the hospital with hematochezia and anemia (Hb of 9 mg/dL, normal levels: 12-15 mg/dL) without hemodynamic instability. Gastroscopy showed erosive antritis and colonoscopy with ileoscopy was normal. The patient was discharged on pantoprazole and iron supplementation. Two weeks latter the patient was admitted with a new episode of hematochezia with hemodynamic instability and a Hb of 6.3 mg/dL. He was transfused three packed blood cells units. Gastroscopy was normal. Colonoscopy yielded blood in the ascending colon and cecum without any mucosal abnormalities. Small amounts of blood were also seen in the terminal ileum without an evident source of bleeding. After profuse washing a 1-mm mucosal defect with a central slightly protruding vessel consistent with a Dieulafoy’s lesion was seen. The lesion spontaneously began to bleed in a pulsating fashion (A). Treatment with argon plasma coagulation (30W) and thermocoagulation using bipolar probe failed to stop the bleeding (B). Finally, a hemoclip was placed resulting in immediate hemostasis. The patient was discharged 4 days after the procedure (C, Video). There were no further episodes of bleeding 6 months afterwards.